How Laser Therapy Can Benefit the Manual Therapist
Contributed by Mark Callanen, PT, DPT, OCS
Unfortunately, the manual therapy world often draws lines in the sand when it comes to treatment approaches. Clinicians tend to define themselves with a particular manual therapy approach and generally don’t give much thought to how a modality might shape their practice. However, best practice usually involves combining various philosophies and evidence based technologies to maximize patient outcomes.
The use of modalities in the orthopedic and sports medicine arenas have historically waxed and waned. It is not uncommon that after a device or technique is introduced to the market, research follows that suggests it has limited efficacy and its popularity in the field fades quickly. Laser technology was not immune to this cycle. Early research regarding laser therapy with lower powered lasers was underwhelming. However, recent advances in equipment and better understanding of photobiomodulation (PBM) has shown that laser therapy is effective in reducing pain1,2,14,15,16,17 and inflammation.1,2,10,11,12,13 It is part of the reason that in February 2017 The American College of Physicians endorsed laser therapy for treatment of chronic low back pain.3
In 2004 laser therapy took a quantum leap forward when the FDA approved the use of Class IV lasers for treating musculoskeletal injuries. Prior to that, most research was based on lower power, Class IIIb lasers which were at worst shown to be ineffective, or at best to have significant clinical limitations. Compared to Class IV lasers, they require longer treatment times and are only effective over smaller areas.4
PBM occurs when an effective dose of light energy is applied to injured tissue. The general mechanism for laser therapy involves stimulation of chromophores on the inner mitochondrial membrane of different cell types that trigger several positive biochemical changes to injured tissue. These changes to musculoskeletal tissue and nerve tissue can improve inflammation,10,11,12,13 decrease pain,1,2,14,15,16,17 and accelerate tissue healing.5,6,7,8,9,10
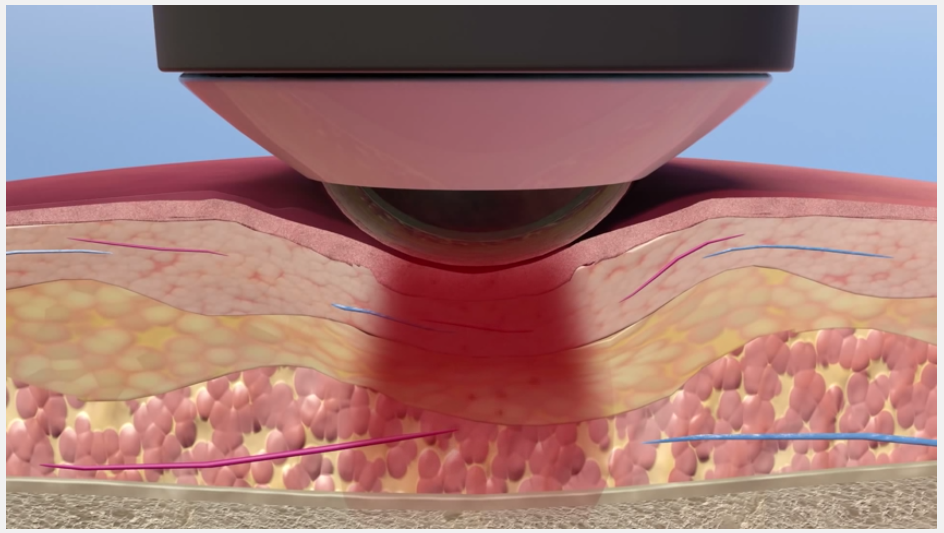
While higher powered lasers make it easier for clinicians to apply appropriate doses of light energy to injured tissue, power is not the only variable that impacts effective dosing. Wavelength is another key variable, and many popular therapy lasers use research-based wavelengths to maximize the ability to energize somatic tissue. Additionally, treatment delivery method is important and can greatly effect outcomes. Delivery system technology such as the patented LightForce massage ball treatment head attachment allow clinicians to directly compress and manipulate tissue while using the laser. This helps minimize scatter and reflection, blanch away unwanted fluid close to the skin surface, and place the source of the laser closer to the intended tissue.
All these factors maximize the energy penetration to deeper tissues. This is important, because if the appropriate level of energy does not reach the injured tissue, PBM will not take place where it is needed, and the treatment will be ineffective.

What does this mean to you the practicing clinician? Deep tissue therapy lasers have the ability to help accelerate plans of care and assist most manual therapy approaches by quickly reducing pain. Clinicians are faced daily with acute and semi-acute presentations that are challenging to treat in early stages due to muscle guarding and subjective complaints associated with inflammation. Laser therapy has analgesic effects that can help with these patients.
When laser is applied in sufficient doses, it has the ability to slow down conduction rates and increase the size of the action potentials in both C and A-delta afferent nerves14,15,16. This can result in quick changes in patients’ pain complaints. This analgesic effect can open the door to more manual options when applied prior to manual treatments.
Additionally, PBM up-regulates anti-inflammatory mediators7,8,9,10,11,12,13 and stimulates growth factors5,6 which will transition patients from the inflammatory phase to the proliferative and remodeling phases of healing more quickly. This will allow for better tolerance of manual techniques and enable active exercises and functional activities to be introduced more quickly into plans of care.
This is a primary reason over 150 Division I and professional training rooms are utilizing LightForce Laser Therapy technology with their injured athletes to optimize their return to sport. If you think your patients could benefit from this advanced technology, regardless of what your manual philosophies might be, please reach out for additional information.
1. Chow et al. Inhibitory Effects of Laser Irradiation on Peripheral Mammalian Nerves and Relevance to Analgesic Effects: A Systematic Review. Photomedicine and Laser Surgery Volume X, Number X, 2011ª Mary Ann Liebert, Inc. Pp. 1–17 DOI: 10.1089/pho.2010.29282. Chow et al. Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials. www.thelancet.com Vol 374 December 5, 2009
3. Amir Qaseem, MD, PhD, MHA; Timothy J. Wilt, MD, MPH; Robert M. McLean, MD; Mary Ann Forciea, MD; for the Clinical Guidelines Committee of the American College of Physicians (*) Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. CLINICAL GUIDELINES |14 FEBRUARY 2017
4. Pryor, B. Smith, J. Laser Therapy Scientific Background. Scientific Report pp 44-49.
5. Benayahu, D, Maltz, L, Oron, U, Stein, A 2005, ‘Low-Level Laser Irradiation Promotes Proliferation and Differentiation of Human Osteoblasts in Vitro’, Photomedicine and Laser Surgery, vol. 23, no. 2, pp. 161-166.
6. Abrahamse, H, Mathope, T, Moore, T, Mvula, B 2008, ‘The effect of low level laser therapy on adult human adipose derived stem cells’, Lasers in Medical Science, vol. 23, no. 3, pp. 277–252.
7. Bansal, H, Dube, A, Gupta, PK 2003, ‘Modulation of macrophage structure and function by low level He–Ne laser irradiation’ Photochemical and Photobiological. Sciences, vol. 2, pp. 851–855.
8. Qin, JZ, Xin, H, Xin, SY, Zeng, H 1992, ‘The activating action of low level helium-neon laser irradiation on macrophages in mouse model’, Laser Therapy, vol. 4, pp. 55–58.
9. Bolton, P, Dyson, M, Young, SR 1990, ‘Effect of light on calcium uptake by macrophages’, Laser Therapy, vol.5, pp. 53–57.
10. Karu, T 1991, ‘Low-Intensity Laser Light Action Upon Fibroblasts and Lymphocytes’, in Calderhead, RG & Ohshiro, T, Progress in Laser Therapy, J. Wiley and Sons, Chichester, New York, Brisbane, Toronto, Singapore, pp.175-180.
11. Greguss, P, Haina, D, Mester, A, Mester, E, Nagylucskay S, Tisza S Waidelich W 1978, ‘Effects of direct laser radiation on human lymphocytes’, Arch Dermatol Res, vol. 263, no. 3, pp. 241-245.
12. Eichler, M, Friedmann, H, Kaplan, D, Lavi, R, Lubart, R, Rickover, O, Shainberg, A, Shneyvays V 2003, ‘Low energy visible light induces reactive oxygen species generation and stimulates an increase of intracellular calcium concentration in cardiac cells’, Journal of Biological Chemistry, vol. 278, pp. 40917-40922.
13. Eichler, M, Friedman, H, Lavi, R, Lubart, R, Shainberg, A 2005, ‘Low-Energy Laser Irradiation Promotes Cellular Redox Activity’, Photomedicine and Laser Surgery, vol. 23, no. 1, pp. 3-9.
14. Alvarez-Leefmans, FJ, Arguelles, CF, Granados-Soto, V 2005, ‘Peripheral and central antinociceptive action of Na+-K+-2Cl- cotransporter blockers on formalin-induced nociception in rats’, Pain, vol. 114, no. 1, pp. 231-238.
15. Friedman, H, Lubart, R 1911, ‘Nonlinear photobiostimulation: the mechanism of visible and infrared laser- induced stimulation and reeducation of neural excitability and growth’, Laser Therapy, vol.3, no. 1, pp. 15-18.
16. Kawatani, M, Matsumoto, I, Sato, T, Takeshige, C, Tsuchiya K 1993, ‘Diode laser irradiation selectively diminishes slow component of axonal volleys to dorsal roots from the saphenous nerve’, Neuroscience Letters, vol. 161, no. 1, pp. 65-68.
17. Wakabayashi, H 1993, ‘Effect of irradiation by semiconductor laser on responses evoked in trigeminal caudal neurons by tooth pulp stimulation’, Lasers in Surgery and Medicine, vol. 13, no. 6, pp. 605-610

Comments