A New Take on Treating Headaches: Can Photobiomodulation Therapy Help?
Contributed by Mark Callanen, PT, DPT, OCS
Treating headaches (HA) can be challenging, and they make up a sizable portion of many practices. Head pain is the 5th leading cause of visits to emergency departments in the U.S. and accounted for 1.2% of all outpatient visits.1 With approximately 300 classifications of different types of HA2, learning how to differentiate and treat this problem challenges even the most experienced clinicians.
Cervicogenic headache (CGHA) is one of the most common and treatable types of HA, accounting for 14-18% of all HA.3 Characteristics of CGHA include unilateral headache that doesn’t change side; pain that is exacerbated with neck movements or abnormal postures; pain produced with pressure applied over the supero-posterior ipsilateral neck; ipsilateral neck, shoulder, or arm pain; and restricted cervical spine range of motion (ROM).4
When inflammation and/or pain is being generated from one or more of the upper 3 cervical segments, it can cause this type of HA.5 CGHA has a very distinct unilateral pattern, often traveling from the occipital area towards the ipsilateral side of the forehead and face due to the involvement of the trigeminal nuclei. Unlike most headaches, it can be reproduced via physical exam. Once CGHA has been confirmed it is then a matter of deciding what treatment to use on the offending segment(s). But what treatment is best?
Any manual treatment that helps improve the segmental mobility of the involved segment(s) will usually help the condition. This can include soft tissue work, mobilization, and/or manipulation. Following up with ROM exercises, postural correction, and using modalities to minimize local pain complaints is standard practice for most clinicians.
 For an even better outcome, you may want to consider adding a tool known as “photobiomodulation therapy” to this manual approach. Also commonly known as “laser therapy”, PBM therapy has been shown to significantly help with chronic and acute cervical pain.6
For an even better outcome, you may want to consider adding a tool known as “photobiomodulation therapy” to this manual approach. Also commonly known as “laser therapy”, PBM therapy has been shown to significantly help with chronic and acute cervical pain.6
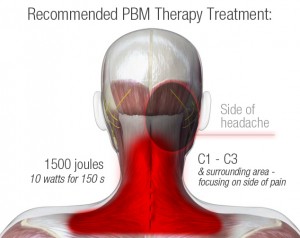
The laser helps the body reduce pain and inflammation via a process known as photobiomodulation.7-10 If applied to the upper cervical area, it has the potential to help patients dealing with CGHA by impacting inflammation, improving cervical muscle endurance, and reducing pain as it relates to peripheral nociception.
PBM has been shown in both in-vitro and in-vivo studies to reduce inflammation by impacting levels of prostaglandin E2, interleukin 1β, and tumor necrosis factor α.11 Animal studies have also confirmed that the anti-inflammatory effects of PBM therapy are similar to pharmacological agents such as celecoxib (Celebrex), meloxicam, diclofenac, and dexamethasone.12,13 Additionally, PBM therapy stands out as an ideal modality choice when treating zygapophyseal joint inflammation due to its ability to deeply penetrate tissue.14,15
Since photobiomodulation promotes increased ATP production in the mitochondria of muscle cells, endurance is significantly improved by laser therapy due to decreases in oxidative stress on muscle tissue.16,17 Additionally, the added ATP production enhances the contractile function of skeletal muscle by attenuating strength loss.18,19 These positive changes in muscle output should help improve reconditioning postural muscles in the neck and upper back as length tension characteristics are being adjusted with corrective exercises and postural cueing.
Finally, the mechanism for delivering pain from the periphery can be impacted with PBM therapy as it inhibits transmission at the neuromuscular junction which has been shown to reduce myofascial pain and trigger points.20,21 Soft tissue dysfunction is commonly associated with pain in the upper cervical spine and HA. Additionally, Aδ and C afferent fibers, which convey peripheral nociception, can have their transmission rates reduced by laser, leading to a reduction in pain perception.6 Slowing peripheral nociception could reduce one of the key drivers of CGHA.
The impact of correctly diagnosing CGHA and isolating the irritable segment(s) in the neck is a critical step in helping these individuals. Having the knowledge and skill to help them is not common place in all out-patient clinics. A growing number of clinics are utilizing PBM therapy with their patients and might find the use of the laser a game changer regarding their approach to CGHA, despite not having the highly developed manual skills to isolate and treat the offending segment.
It is easy to see how PBM therapy could help current protocols by reducing local inflammation, improving muscle function of the surrounding muscles, and reducing the nociceptive abilities of the nerves involved with CGHA. Even if you are a clinician with the skill to provide the perfect manual treatment to the upper cervical spine, any one of the characteristics listed above could further improve a CGHA outcome. Imagine if you could add all three…
Patients dealing with both acute and chronic neck pain have already been shown to benefit from PBM6, so why shouldn’t people dealing with CGHA? If your practice treats patients with neck related disorders, you might want to consider a therapeutic laser as the next modality you add to your clinic, regardless of the manual tools that are at your disposal.
References
1. Smitherman TA, Burch R, Sheikh H, Loder E. The prevalence, impact, and treatment of migraine and severe headaches in the United States: a review of statistics from national surveillance studies. Headache. 2013 Mar;53(3):427-36. 2. Heachache Classification Subcommittee of the Internoational Headache Society. The international classification of headache disorders, 2nd Edition. Cephalagia 2004; 24: suppl 1. 3. G. Zito, G. Jull , I. Story. Clinical tests of musculoskeletal dysfunction in the diagnosis of cervicogenic headache. Manual Therapy 11 (2006) 118–129. 4. Sjaastad O, Fredriksen TA, Pfaffenrath V. Cervicogenic headache: diagnostic criteria. the cervicogenic headache international study group. Headache. 1998;38:442–5. 5. Lord S, Bogduk N. The cervical synovial joints as sources of posttraumatic headache. Journal of Musculoskeletal Pain 1996;4:81–94. 6. Chow, RT. Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomized placebo or active-treatment controlled trials. Lancet 2009; 374: 1897–908. 7. Sattayut S, Hughes F, Bradley P. 820nm gallium aluminium arsenide laser modulation of prostaglandin E2 production in interleukin I stimulated myoblasts. Laser Therapy 1999; 11: 88–95. 8. Sakurai Y, Yamaguchi M, Abiko Y. Inhibitory eff ect of low-level laser irradiation on LPS-stimulated Prostaglandin E2 production and cyclooxygenase-2 in human gingival fibroblasts. Eur J Oral Sci 2000; 1081: 29–34. 9. Aimbire F, Albertini R, Pacheco MTT, et al. Low-level laser therapy induces dose-dependent reduction of TNFα levels in acute inflammation. Photomed Laser Surg 2006; 24: 33–37. 10. Bjordal JM, Johnson MI, Iverson V, Aimbire F, Lopes-Martins RAB. Photoradiation in acute pain: a systematic review of possible mechanisms of action and clinical effects in randomized placebocontrolled trials. Photomed Laser Surg 2006; 24: 158–68. 11. Bjordal JM, Lopes-Martins RAB, Iversen VV. A randomised, placebo controlled trial of low level laser therapy for activated achilles tendinitis with microdialysis measurement of peritendinous prostaglandin E2 concentrations. Br J Sports Med 2006; 40: 76–80. 12. Campana V, Moya M, Gavotto A, et al. The relative effects of He-Ne laser and meloxicam on experimentally induced inflammation. Laser Therapy 1999; 11: 36–42. 13. Albertini R, Aimbire F, Correa FI, et al. Eff ects of diff erent protocol doses of low power gallium–aluminum–arsenate (Ga–Al–As) laser radiation (650 nm) on carrageenan induced rat paw oedema. J Photochem Photobiol B 2004; 27: 101–07. 14. Enwemeka C. Attenuation and penetration of visible 632・8nm and invisible infrared 904nm light in soft tissues. Laser Therapy 2001; 13: 95–101. 15. Gursoy B, Bradley P. Penetration studies of low intensity laser therapy (LILT) wavelengths. Laser Therapy 1996; 8: 18. 16. Leal Junior EC, Lopes-Martins RA, Vanin AA, et al. Effect of 830 nm low-level laser therapy in exercise-induced skeletal muscle fatigue in humans. Lasers Med Sci 2009; 24: 425–31. 17. Leal Junior EC, Lopes-Martins RA, Dalan F, et al. Effect of 655-nm Low-Level Laser Therapy on Exercise-Induced Skeletal Muscle Fatigue in Humans. Photomed Laser Surg 2008; 26: 419–24. 18. Kelly A. Larkin-Kaiser, KA. Near-Infrared Light Therapy to Attenuate Strength Loss After Strenuous Resistance Exercise. Journal of Athletic Training 2015;50(1):45–50. 19. Nampo, FK. Low-level phototherapy to improve exercise capacity and muscle performance: a systematic review and meta-analysis. Lasers Med Sci (2016) 31:1957–1970. 20. Nicolau R, Martinez M, Rigau J, Tomas J. Neurotransmitter release changes induced by low power 830nm diode laser irradiation on the neuromuscular junction. Lasers Surg Med 2004; 35: 236–41. 21. Nicolau RA, Martinez MS, Rigau J, Tomas J. Effect of low power 655nm diode laser irradiation on the neuromuscular junctions of the mouse diaphragm. Lasers Surg Med 2004; 34: 277–84.
Comments