THE SCIENCE BEHIND HOW LASER THERAPY WORKS
HOW DOES LASER THERAPY WORK?
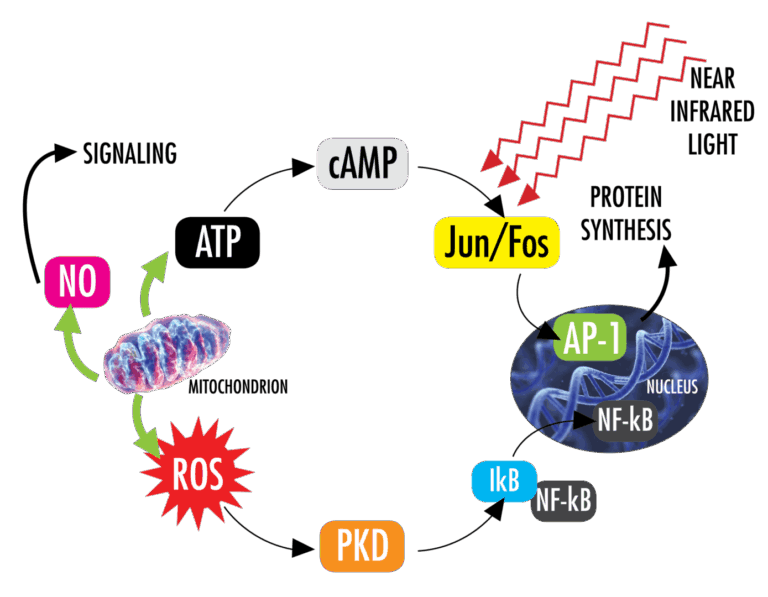
Laser therapy is a medical treatment that uses focused light to stimulate a process called photobiomodulation (PBM means photobiomodulation). During PBM, photons enter the tissue and interact with the cytochrome c complex within mitochondria. This interaction triggers a biological cascade of events that leads to an increase in cellular metabolism, which can decrease pain as well as accelerate the healing process.
Photobiomodulation therapy is defined as a form of light therapy that utilizes non-ionizing light sources, including lasers, light emitting diodes, and/or broadband light, in the visible (400 – 700 nm) and near-infrared (700 – 1100 nm) electromagnetic spectrum. It is a nonthermal process involving endogenous chromophores eliciting photophysical (i.e., linear and nonlinear) and photochemical events at various biological scales. This process results in beneficial therapeutic outcomes including but not limited to the alleviation of pain, immunomodulation, and promotion of wound healing and tissue regeneration. The term photobiomodulation (PBM) therapy is now being used by researchers and practitioners instead of terms such as low level laser therapy (LLLT), cold laser, or laser therapy.
The fundamental principles that underpin photobiomodulation (PBM) therapy, as currently understood in the scientific literature, are relatively straightforward. There is consensus that the application of a therapeutic dose of light to impaired or dysfunctional tissue leads to a cellular response mediated by mitochondrial mechanisms. Studies have shown that these changes can impact pain and inflammation, as well as, tissue repair.
PHOTOBIOMODULATION PROCESS
Stimulate Cytochrome C
The primary target for the photobiomodulation process is the Cytochrome C complex, which is found in the inner membrane of the cell mitochondria. Cytochrome C is a vital component of the electron transport chain that drives cellular metabolism.
Increase Production of ATP (Energy)
As light is absorbed by Cytochrome C oxidase (COX), it stimulates the electron transport chain to increase the production of adenosine triphosphate (ATP) within the mitochondria. When tissue is damaged, the production of ATP in the cell is impaired which slows down the metabolism of the cell as a protective mechanism. PBM helps restore the oxidative process which helps restore normal cellular function.
Increase NO and ROS Activity
In addition to ATP, laser stimulation also produces free nitric oxide (NO) and modulates reactive oxygen species (ROS). NO is a powerful vasodilator and an important cellular signaling molecule involved in many physiological processes. ROS have been shown to affect many important physiological signaling pathways including the inflammatory response. Together, increased NO and improved ROS levels provide an environment for faster signaling, resulting in decreased inflammation.
Restore Cellular Energy Balance
PBM helps restore normal cellular function which helps prevent apoptosis (cell death). This helps reduce inflammation, edema, and hastens the tissue repair process.
REACHING TARGET TISSUE
For PBM to occur, light needs to reach the mitochondria of the damaged target tissue. When laser therapy is applied to the surface of the skin the best results are achieved when a sufficient amount of light (number of photons) reaches the target tissue. There are a number of factors that can help maximize the light that reaches the target tissue, including:
• Light Wavelength
• Minimizing Unwanted Absorption
• Power
• Reducing Reflections
WHAT WAVELENGTHS OF LIGHT ARE THE BEST FOR PHOTOBIOMODULATION (PBM)?
As opposed to white light, which contains a broad range of wavelengths, laser light is monochromatic which means it contains one wavelength. The unit used to measure wavelength is a nanometer (nm). Much research has been done to investigate how melanin, blood, fat and water absorb light, and this has led researchers to define a window or range of wavelengths through which light can penetrate biological tissue. This window is referred to as the optical or therapeutic window.

This graph shows water absorption on a linear scale. LightForce® lasers utilize both 810 and 980 nm wavelengths due to their ability to be preferentially absorbed by musculoskeletal tissues. These wavelengths also minimize the interference of melanin which has an affinity for shorter wavelengths as well as the impact of water within the body which preferentially absorbs longer wavelengths. Energy that is absorbed by melanin or water in the body is energy that is lost at the target tissue.
POWER
The brightness of a laser is defined in a similar fashion as other light sources, in Watts (W) or milliwatts (mW).
Power influences photobiomodulation therapy in a number of ways. When energy is imparted to the body, it is measured in Joules. Joules is the product of power (Watts) x time (seconds). By definition, higher power allows Joules to be delivered to tissue in less time. This allows larger areas and deeper tissues to be treated more quickly. Recent research has also shown that higher power density, referred to as irradiance, can have profound effects on reducing pain in minutes. All of these factors are clinically desirable.
Early therapeutic lasers had very low powers (less than 0.5 W) and very small beam areas (or spot sizes); consequently, early studies were often disappointing because the low powers were not able to provide a sufficient number of photons to significantly impact injured cells. The FDA classifies lasers according to their output power and risk to the eye. These classes include IIa (bar code scanner), IIIa (laser pointer), IIIb (industrial and therapy lasers <499 mW), and Class IV (all lasers >500 mW). In December 2003, the FDA approved the first Class IV laser for the relief of minor muscle and joint pain. In October 2006, LiteCure, LightForce®’s parent company, was formed and FDA clearance for the LCT-1000, a Class IV medical therapy laser, was granted in February 2007. LightForce® has been providing Class IV lasers for the US market, and growing global market, ever since.
LightForce® lasers not only have the ability to deliver higher power for various conditions, but they also incorporate delivery systems that can efficiently treat tissue in a way that is comfortable to the patient. Simply stated, injured tissue requires threshold levels of light (photons) to be delivered in order to have a therapeutic effect. Hundreds of scientific studies on photobiomodulation therapy have been done in vivo and have characterized the dosages needed to achieve a cellular response to light. The required levels of energy needed to impact tissue during in vivo studies is significantly higher due to the loss of energy that takes place as light travels through tissue. Examples of these losses include the impact of melanin in the skin, extra cellular water, and other molecules in the plasma that might absorb photonic energy. LightForce® has participated in multiple double-blind photobiomodulation therapy studies in order to help quantify these differences and deliver protocols that are safe and effective.
Infrared images illustrate the amount of light seen on the back of the hand when laser light is applied to the palm at 1 watt, 5 watts, and 10 watts of power.
The greater the power, the larger the number of photons that will be delivered to deeper tissues during photobiomodulation therapy. With the higher power lasers, it is possible to not only apply the benefits of PBM superficially, but it is also possible to treat a greatly expanded range of conditions by delivering a clinically effective quantity of photons to cells deep within tissue.

Learn more about how power impacts photobiomodulation therapy. >
READY TO LEARN MORE
Read about the latest science in photobiomodulation therapy. >
Watch the webinar: What is Laser Therapy? >