Laser Therapy FAQ 3 – How is Photobiomodulation Therapy Different from Therapeutic Ultrasound?

Contributed by Mark Callanen, PT, DPT, OCS
Photobiomodulation therapy (also known as laser therapy) is a nonthermal, photochemical process that results in beneficial therapeutic outcomes, including the alleviation of pain and inflammation, immunomodulation, and promotion of wound healing and tissue regeneration. It also promotes muscle relaxation and increased local circulation. While this sounds similar to the effects of ultrasound, the two modalities are actually quite different.
Therapeutic ultrasound works by a piezoelectric effect. A vibrating crystal in the head creates cavitation in tissue via sound waves. This cavitation produced in therapeutic ultrasound machines causes friction among water molecules and in turn creates heat in the tissue. This warming effect promotes local vasodilation.
When deep tissue lasers are used, there is often minor heating at the epidermis, as melanin and hair will absorb light energy. While the minor heating can help relax muscles and decrease pain, the heat sensed at the skin is not what creates the improvements in microcirculation and local vasodilation – these effects result from a process called photobiomodulation (PBM).1,2
Local perfusion increases after specific wavelengths of light reach the inner mitochondrial membrane of injured cells and excite the chromophore Cytochrome C. When energized adequately, activated Cytochrome C oxidase frees up bound nitrous oxide (NO), which improves vasodilation in the local area and promotes healing.3 In addition to freeing up NO, there are a host of other beneficial cellular interactions that take place during photobiomodulation that positively influence the inflammatory cascade and improve tissue healing by impacting the mitochondria directly.3
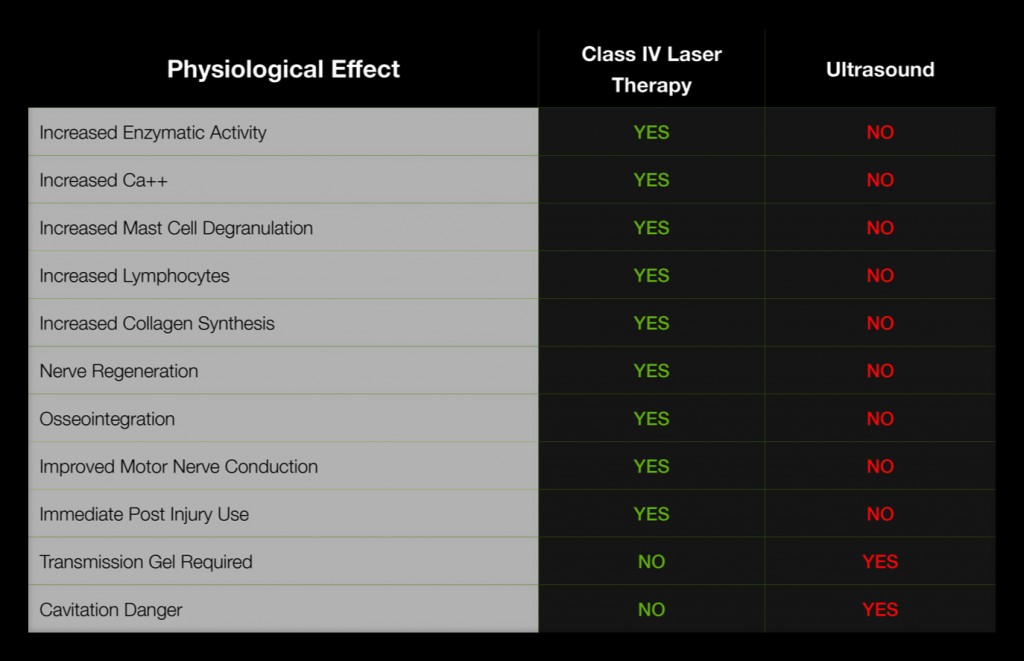
The chart below shows several differences between the laser and ultrasound modalities. Given that laser’s mechanism of action impacts the metabolism of the mitochondria and ultrasound does not, the influence the two modalities has on tissue(s) is quite different.
An added benefit of PBM therapy is that it can be used over metal implants, while ultrasound cannot. Since light is simply reflected off metal, use over total joints is not a contraindication. Given laser’s ability to have positive effects on inflammation and pain, it is the ideal modality to use on post-operative total joint patients with pain and swelling.
As research continues to build and better outcomes are achieved consistently, health professionals are increasingly viewing PBM therapy as a clinical asset worth investing in. Unlike ultrasound, laser’s ability to quickly impact pain, inflammation, and tissue repair make it a very versatile modality – one that clinicians find themselves reaching for again and again. So if you are looking at bringing a modality into into your practice, take a look at deep tissue therapy lasers – the only thing you will regret is not getting one sooner.
1. Mrowiec J 1997, ‘Analgesic effect of low-power infrared laser radiation in rats’, Proc SPIE, vol. 3198,no. 83, pp. 83-89. 2. Asagai, Y. 2000, “Thermagraphic study of low level laser for acute phase injury”, Las Ther, vol 12. pp 31-33. 3. Chris E. Stout, Matt Kruger and Jeffrey Rogers, (Eds)- © 2011 Bentham Science Publishers Ltd. Current Perspectives in Clinical Treatment & Management in Workers’ Compensation Cases, 2011, 15: 191-2.
Comments